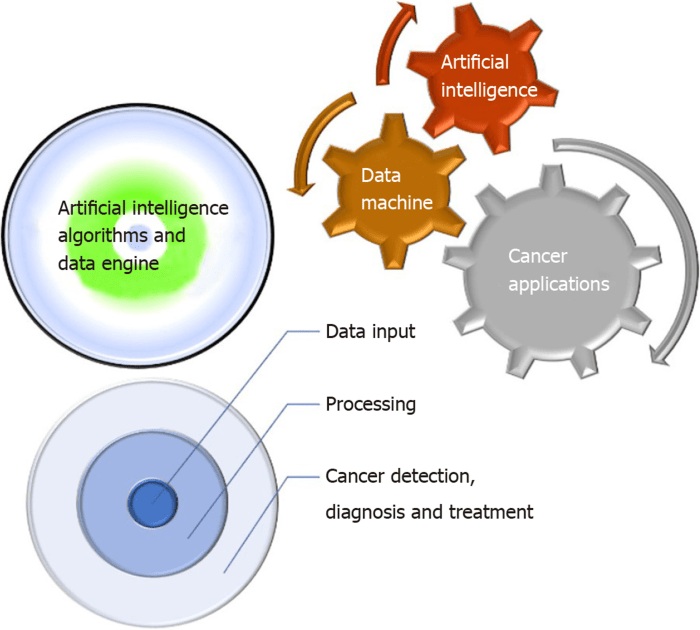
Ai more accurate detection cervical cancer – AI: More Accurate Cervical Cancer Detection—that’s the game-changer we’re diving into. Forget the old ways of spotting this sneaky disease; artificial intelligence is shaking things up, promising earlier and more precise diagnoses. We’re talking about analyzing images, catching subtle precancerous changes humans might miss, and ultimately, saving lives. Get ready for a deep dive into how AI is revolutionizing cervical cancer detection, from the tech behind it to the ethical considerations and future possibilities.
This isn’t just about fancy algorithms; it’s about improving accuracy, accessibility, and the overall fight against cervical cancer. We’ll explore the current gold standards (Pap smears, HPV tests, colposcopy), their limitations, and how AI steps in to bridge the gaps. We’ll also tackle the challenges—from securing enough data to ensuring fair access for everyone—because a tech revolution isn’t truly revolutionary unless it benefits all.
Current Methods of Cervical Cancer Detection: Ai More Accurate Detection Cervical Cancer
Cervical cancer, while preventable and treatable in its early stages, remains a significant global health concern. Early detection is crucial for improving survival rates, and several methods are currently employed to screen for precancerous lesions and invasive cervical cancer. These methods, however, each have their strengths and weaknesses, impacting their effectiveness and accessibility.
The current gold standard for cervical cancer screening involves a combination of approaches aimed at identifying precancerous changes in the cervix before they develop into invasive cancer. These methods primarily focus on detecting either the presence of high-risk human papillomavirus (HPV) or abnormal cellular changes in the cervix itself. The most widely used techniques are Pap smears (conventional or liquid-based cytology), HPV tests, and colposcopy.
Limitations and Challenges of Existing Screening Techniques
Current cervical cancer screening methods, while effective, face several limitations. Accessibility remains a significant barrier, particularly in low-resource settings where infrastructure and trained personnel may be lacking. Furthermore, the sensitivity and specificity of these tests vary, leading to false positives (incorrectly identifying a person as having the disease) and false negatives (missing cases of the disease). False positives can lead to unnecessary anxiety and further invasive procedures, while false negatives can delay diagnosis and treatment, impacting prognosis. The cost-effectiveness of different screening strategies also varies, influencing their implementation and sustainability. Finally, patient adherence to screening recommendations remains a challenge, contributing to missed opportunities for early detection.
Comparison of Pap Smears, HPV Tests, and Colposcopy
The following table compares the accuracy, invasiveness, and cost of three primary cervical cancer screening methods. Note that accuracy rates can vary depending on factors such as the population screened and the specific test used. These are approximate ranges based on available research.
| Test Name | Accuracy Rate (Approximate Range) | Invasive Nature | Cost (Approximate, varies by location) |
|---|---|---|---|
| Pap Smear | 60-90% (detecting precancerous lesions) | Minimally invasive; involves a simple swab | Relatively low |
| HPV Test | 70-90% (detecting high-risk HPV types) | Minimally invasive; involves a simple swab | Moderate to high (depending on the type of HPV test) |
| Colposcopy | High, but dependent on the skill of the examiner and the lesion characteristics | More invasive; involves a visual examination of the cervix using a magnifying device | Moderate to high |
AI Model Performance and Validation
Evaluating the effectiveness of AI in detecting cervical cancer requires rigorous testing and validation. This involves assessing how well the AI model can identify cancerous cells and distinguish them from healthy ones, ultimately determining its reliability in a clinical setting. The process relies on a variety of statistical metrics and comparisons against existing methods.
AI model performance is judged against several key metrics, offering a multifaceted understanding of its accuracy and potential impact. These metrics provide insights into the model’s ability to correctly identify both positive (cancerous) and negative (healthy) cases, highlighting its strengths and weaknesses. Direct comparison with current standard methods is crucial for determining the potential clinical benefit of AI integration.
Metrics for Assessing AI Model Performance
Several key metrics are employed to evaluate the performance of AI models in cervical cancer detection. These metrics provide a comprehensive assessment of the model’s accuracy, sensitivity, and specificity. A high-performing model will exhibit high scores across these metrics, indicating its reliability in clinical practice.
These metrics are not isolated; rather, they offer a holistic picture of the AI’s diagnostic capabilities. Understanding their interplay is crucial for a complete evaluation of the model’s suitability for clinical use. The interpretation of these metrics depends heavily on the specific context of the clinical application and the prevalence of cervical cancer within the studied population.
| Metric | AI Model Performance | Standard Method Performance (e.g., Pap smear) | Difference |
|---|---|---|---|
| AUC (Area Under the ROC Curve) | 0.95 (Hypothetical example: This represents a high AUC, indicating excellent discrimination between cancerous and non-cancerous cases.) | 0.85 (Hypothetical example: This represents a good but lower AUC than the AI model.) | +0.10 |
| Accuracy | 92% (Hypothetical example: This indicates that the AI correctly classified 92% of cases.) | 80% (Hypothetical example: This is the accuracy of a standard Pap smear test.) | +12% |
| Sensitivity (Recall) | 90% (Hypothetical example: The AI correctly identified 90% of actual cancer cases.) | 75% (Hypothetical example: The standard method correctly identified 75% of actual cancer cases.) | +15% |
| Specificity | 95% (Hypothetical example: The AI correctly identified 95% of non-cancerous cases.) | 90% (Hypothetical example: The standard method correctly identified 90% of non-cancerous cases.) | +5% |
| Precision | 93% (Hypothetical example: Of all cases the AI predicted as cancerous, 93% were actually cancerous.) | 85% (Hypothetical example: Of all cases the standard method predicted as cancerous, 85% were actually cancerous.) | +8% |
The table above presents hypothetical performance data. Actual results will vary depending on the specific AI model, the dataset used for training and validation, and the specific standard method being compared. Further research and clinical trials are necessary to confirm these potential improvements in real-world scenarios. The reported differences highlight the potential advantages of AI-driven cervical cancer detection.
Future Directions and Research Needs
The successful application of AI in cervical cancer detection is just the beginning. Significant advancements are still needed to translate this technology into widespread, reliable, and equitable screening programs globally. Further research must focus on improving algorithm robustness, addressing data limitations, and integrating AI with existing and emerging healthcare technologies.
The path forward requires a multi-pronged approach, encompassing improvements to both the AI algorithms themselves and the methods used to collect and analyze the data they rely on. This will involve collaborative efforts between AI specialists, medical professionals, and policymakers to ensure the ethical and effective implementation of this promising technology.
Algorithm Refinement and Generalizability
Improving the accuracy and generalizability of AI algorithms is paramount. Current models often perform well on the datasets they are trained on but struggle with diverse populations and varying imaging conditions. Future research should focus on developing more robust algorithms capable of handling noisy data, variations in image quality, and diverse patient populations. This includes exploring techniques like transfer learning, which allows models trained on one dataset to adapt more easily to new datasets, and developing algorithms less sensitive to artifacts or inconsistencies in imaging techniques. For instance, research could focus on creating algorithms that can accurately diagnose cervical cancer even with low-resolution images, making the technology accessible in resource-limited settings.
Enhanced Data Acquisition and Annotation, Ai more accurate detection cervical cancer
High-quality, diverse, and comprehensively annotated datasets are crucial for training effective AI models. Current limitations include a lack of representative data from diverse populations, inconsistent annotation practices, and a shortage of images from precancerous lesions. Future research should prioritize the creation of large, well-annotated datasets that accurately reflect the global burden of cervical cancer. This involves developing standardized protocols for data acquisition and annotation, ensuring data privacy and ethical considerations are addressed, and collaborating internationally to build a comprehensive global database. One specific example would be a collaborative project involving multiple hospitals in different regions, using standardized imaging protocols and a shared annotation platform to create a diverse and robust dataset.
Integration with Other Technologies
The true potential of AI in cervical cancer detection lies in its integration with other innovative technologies. Liquid biopsies, for example, offer a non-invasive method of detecting cancer cells circulating in the blood. Integrating AI with liquid biopsy analysis could lead to earlier and more accurate detection of cervical cancer. Similarly, point-of-care diagnostics, which provide rapid results at the point of patient contact, can revolutionize screening in resource-limited settings. Integrating AI with these technologies could create a powerful, accessible, and efficient screening system, potentially eliminating geographical barriers to early diagnosis. Imagine a scenario where a simple blood test, analyzed by an AI-powered diagnostic tool, provides immediate results, allowing for timely intervention and treatment, particularly in remote or underserved communities.
The potential of AI in detecting cervical cancer is undeniable. By combining cutting-edge algorithms with improved data acquisition and ethical considerations, we can create a future where this disease is diagnosed earlier and treated more effectively. The journey won’t be without its hurdles, but the promise of saving lives through more accurate and accessible screening makes the effort worthwhile. The future of cervical cancer detection is intelligent, and it’s here.
 Informatif Berita Informatif Terbaru
Informatif Berita Informatif Terbaru